The bilirubin urine test is a laboratory test to measure the amount of bilirubin in urine. Urine bilirubin is also called bilirubinuria. A bilirubin urine test is a part of urinalysis that is usually performed by a routine urine dipstick test(1).
It indicates the amount of conjugated or direct bilirubin in the urine.
Usually, urine samples do not have bilirubin in them. So, the presence of bilirubin in urine tests helps diagnose and detect liver diseases very early, even before jaundice is appreciated clinically(1,2).
The abnormal bilirubin level is dangerous, especially in newborn babies, which causes brain damage and disability. It is a diagnostic tool for diseases like blood hemolysis or liver disorders.
What is Bilirubin?
Bilirubin is a greenish-yellow colored pigment that is formed by the normal breakdown of hemoglobin after red blood cell destruction(3).
The human body produces almost 4 mg/kg of bilirubin through the catabolism of RBCs (80-85%) and by ineffective erythropoiesis or the breakdown of muscle myoglobin (15-20%).
Red blood cells have an average lifespan of almost 120 days. After that, they are destroyed by our natural body mechanism called the reticuloendothelial system, particularly in the bone marrow, spleen, and liver.
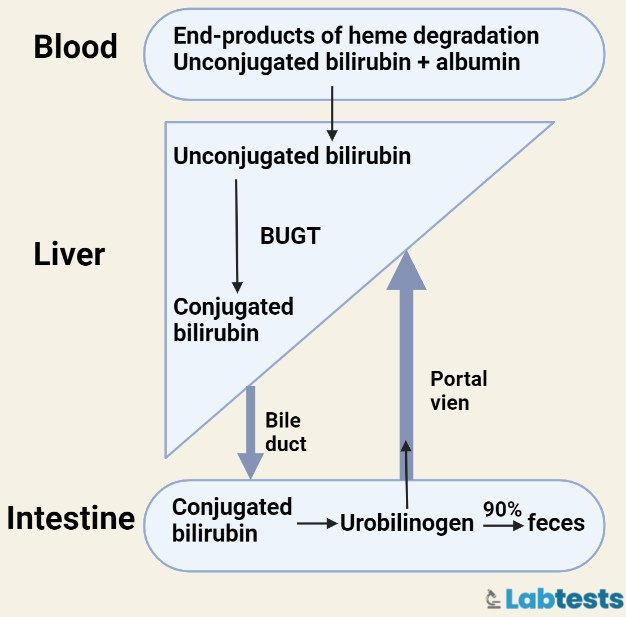
The breakdown of old red blood cells through the spleen and bone marrow is responsible for the formation of bilirubin (See below in Figure 1).
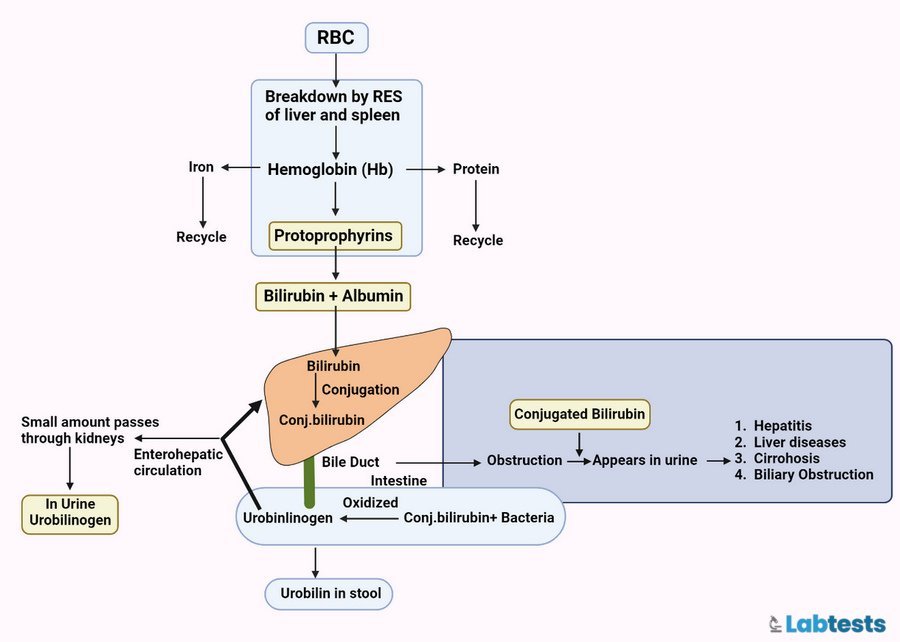
Bilirubin binds to albumin through non-covalent linkage and is transported to the liver when it conjugates. It is then stored in the gallbladder as bile. Bilirubin is considered a waste product, and our body has to get rid of it.
It’s present in the human body in either direct/conjugated bilirubin or indirect/unconjugated bilirubin. Bilirubin is an antioxidant that is oxidized to biliverdin, which is then reduced to regenerate bilirubin.
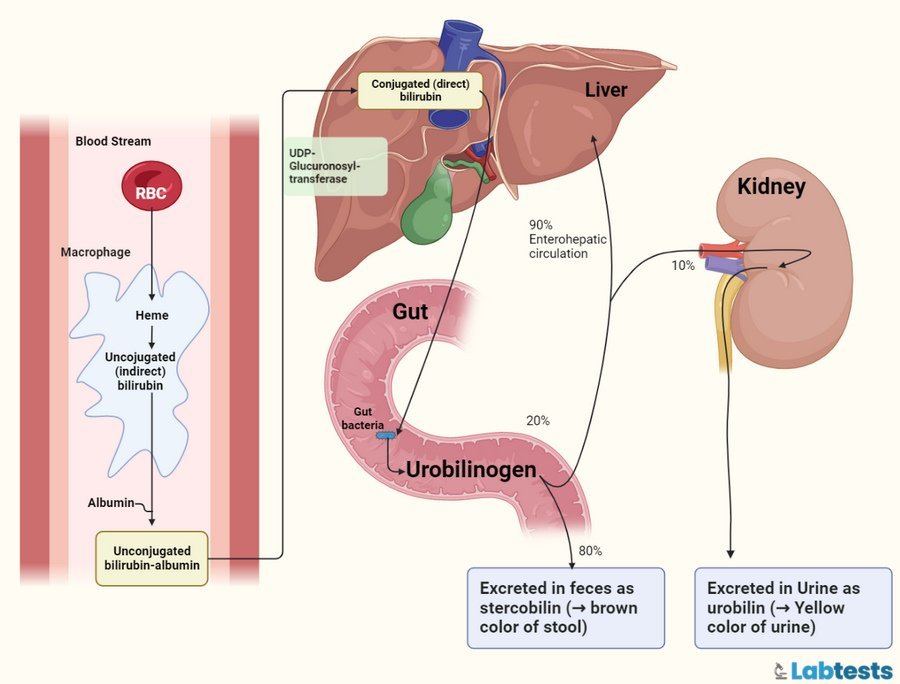
Image created with Biorender
Degradation of Heme
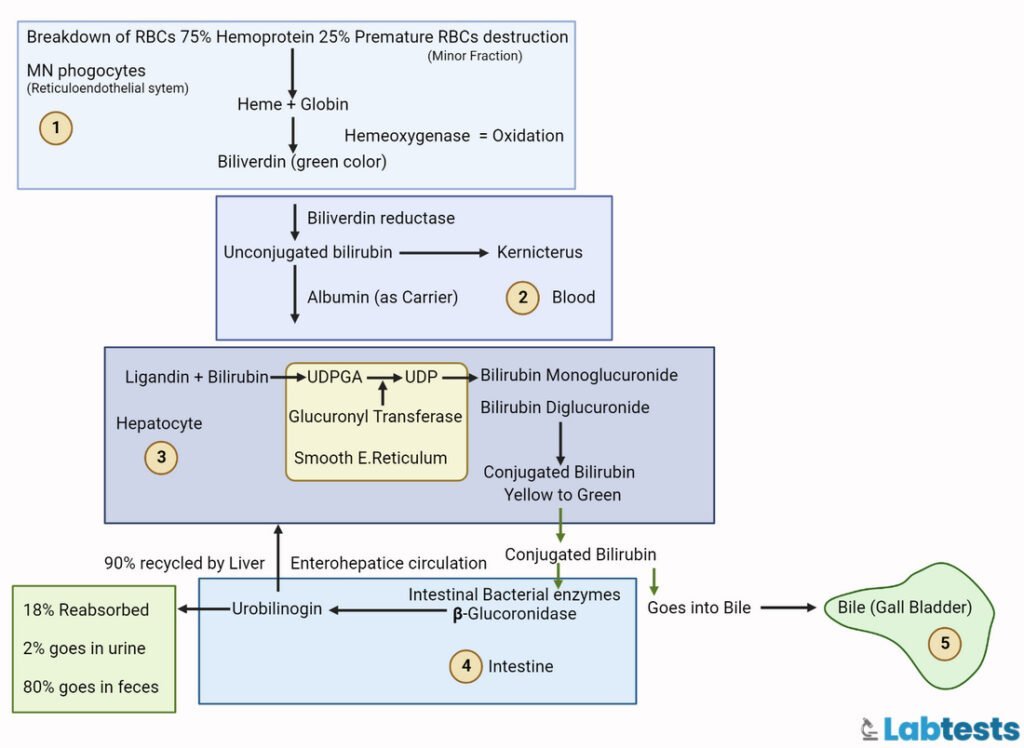
Degradation of heme is a step-wise process. It is described in the following (see also Figure 3 and 3)
Step 1: Fragile or senescent RBCs are a major source of heme. Heme breakdown occurs in the reticuloendothelial system (spleen, tissue macrophages, and liver)
Step 2: Heme is converted to Biliverdin
Step 3: Biliverdin is converted to Unconjugated bilirubin
Step 4: Unconjugated bilirubin binds to albumin protein and is transported to Liver through bloodstream
Step 5: Bilirubin is taken up by the liver and converted to Conjugated bilirubin
Step 6: Conjugated bilirubin is secreted into bile
Step 7: Bile is then stored in the gallbladder or excreted to small Intestine
Step 8: In the small intestine almost 50% of the conjugated bilirubin is converted to urobilinogen (glucuronate is removed by bacteria)
Step 9: Some of the urobilinogen enters the portal blood. Some of the urobilinogen is oxidized by intestinal bacteria and is converted to stercobilin which is of brown color.
Step 10: 5% of the urobilinogen is transported to the kidneys. Urobilinogen is converted to urobilin (Urobilin is yellow in color and gives characteristic color to the urine).
Conjugation of Bilirubin
The conjugation of bilirubin is mandatory to make it water-soluble. Conjugation helps in the excretion of bilirubin into bile. Bilirubin produced as an end product of RBCs metabolism is in the form of indirect or unconjugated bilirubin.
This is transported to the liver via blood. Where it binds to glucuronic acid by uridine-diphosphoglucuronic glucuronosyltransferase (UDPGT) enzyme (see below in figure 4).
Conjugated bilirubin is stored as bile in the gallbladder(9). The size of the molecule also increases with conjugation. Conjugation makes the bilirubin hydrophilic which prevents it from being passively reabsorbed by the mucosa of the small intestine. In this way, conjugation promotes the elimination of toxic metabolites.
Normal range of bilirubin(7)
| Total serum bilirubin | 0.3 to 1.2 mg/dL |
| Direct or conjugated bilirubin | Less than 0.3 mg/dL |
| Indirect or unconjugated bilirubin | Less than 1.1 mg/dL |
Types of Bilirubin
1. Total bilirubin
Both direct and indirect bilirubin are called total bilirubin.
Its reference range is 0.2 to 1.0 mg/dL (serum).
2. Direct bilirubin
Conjugated form of bilirubin is called direct bilirubin. It is water soluble.
Its reference range is 0 to 0.2 mg/dL (serum).
3. Indirect bilirubin
Unconjugated form of bilirubin is called indirect or free bilirubin. It is soluble in fat and insoluble in water. It binds with the protein called albumin. Albumin-bound indirect albumin does not appear in urine because it’s water-insoluble.
Its reference range is 0.2 to 0.8 mg/dl (serum).
Difference between Conjugated and Unconjugated bilirubin
| Conjugated bilirubin | Unconjugated bilirubin |
|---|---|
| It is water soluble | It is water-insoluble |
| Less amount is attached with albumin. | Mostly attached with albumin. |
| It’s less toxic | It’s toxic, especially to the brain. |
| Significantly accumulates in the post-hepatic type of jaundice. | Significantly accumulates in the pre-hepatic type of jaundice. |
| Excreted in through urine. | Can’t be excreted through urine. |
What is Jaundice?
Jaundice is a medical condition in which the bilirubin level (conjugated, unconjugated, or both) is so high in the blood that it causes yellowish discoloration of the skin, nail beds, mucous membranes, and sclera (whites of the eyes) (see in figure 5).
The other name for jaundice is icterus. Jaundice appears clinically when the bilirubin concentration increases up to three times normal.

Types of Jaundice
There are three types of jaundice
1. Pre-hepatic jaundice
- Pre-hepatic jaundice is due to the accumulation of unconjugated or indirect bilirubin.
- Liver can conjugate almost 3000 mg of bilirubin in a day but the human body produces only 300 mg in a day.
- If there is massive lysis of RBCs, the level of unconjugated bilirubin increases and causes jaundice, because the liver can’t conjugate bilirubin so fast.
- Unconjugated bilirubin level is elevated due to pre-hepatic reasons like malaria, breakdown of red blood cells, and some genetic diseases like thalassemia, spherocytosis, G6PD deficiency, heart failure, and Pyruvate kinase deficiency.
2. Hepatic jaundice
- Hepatic jaundice is due to the accumulation of unconjugated or indirect bilirubin.
- Damage to hepatocytes decreases conjugation and leads to the accumulation of unconjugated bilirubin.
- Unconjugated bilirubin level is elevated due to hepatic diseases like hepatitis (acute or chronic ), drug-induced hepatitis, cirrhosis of the liver, and alcoholic liver disease.
- Some other reasons are primary biliary cirrhosis, neonatal jaundice, and genetic disorders like Gilbert’s syndrome or Crigler-Najjar syndrome (6).
3. Post-hepatic jaundice
- Post-hepatic jaundice is due to an interruption in the excretion of bile from the biliary system that leads to the accumulation of conjugated bilirubin.
- Some of the reasons are gallstones getting stuck in the common bile duct, cholangiocarcinoma, strictures of the common bile duct, tumors in the head of the pancreas, biliary atresia, and pancreatitis.
The specimen used for bilirubin urine test
- The sample of the urine should be freshly voided.
- It should be examined immediately after collection, i.e., within two hours of voiding.
- The urine sample should not be exposed to sunlight because sunlight will oxidize bilirubin to biliverdin, and biliverdin is not detected by the reagents we use in tests.
Tests for Urine Bilirubin
The following methods are used to detect bilirubin in the urine sample. The dipstick method impregnated with Diazo reagent is the most commonly used.(8)
1. Harrison’s or Fouchet’s Test
Bilirubin is precipitated with barium chloride and is oxidized to biliverdin with the help of Fouchet’s reagent. Color will turn green due to the formation of biliverdin. Barium sulfate will form when barium chloride is added to the urine (see figure 6 below).
The procedure of the Fouchet’s Test is
- Take a urine sample, add 5 ml of a 10% barium chloride solution, and mix.
- Leave it for a few minutes.
- Then use a small filter paper for filtration.
- Place Fouchet’s reagent on filter paper.
- The reaction will be positive if the color changes from blue to green.
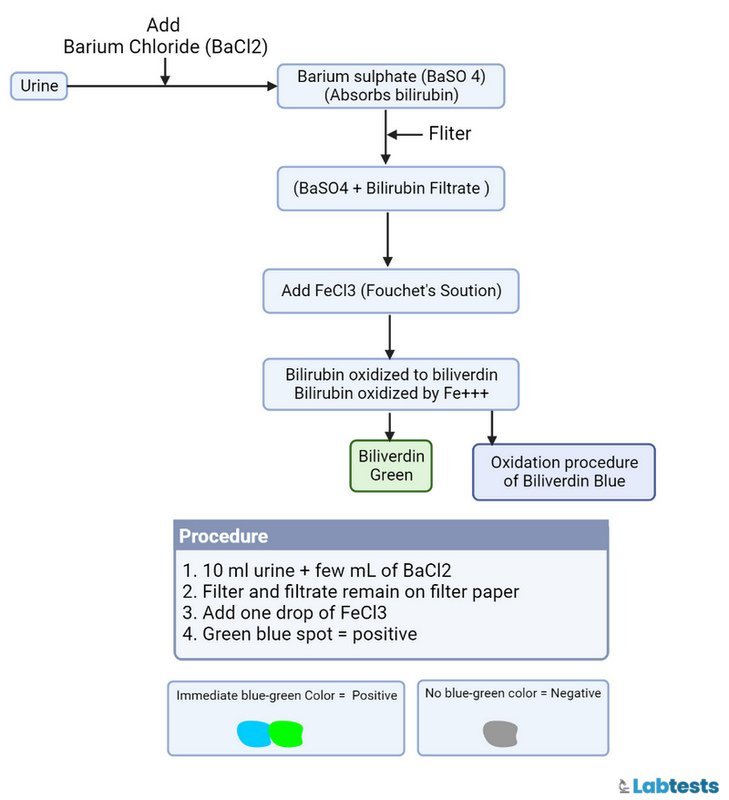
2. Barium chloride Filter Paper Method
This test is modified by Harrison’s test. The procedure of the Barium chloride filter paper method is
- Take a urine sample and dip a strip of barium chloride paper perpendicularly.
- Add Fouchet’s Reagent.
- The green color indicates the test is positive.
- Color other than green or no color shows the test is negative.
3. Diazotization Tests for Bilirubin(4)
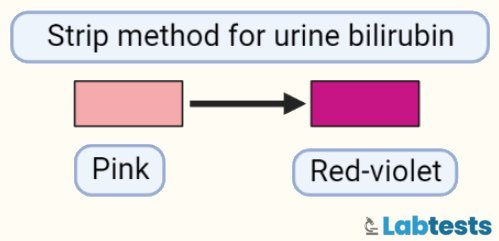
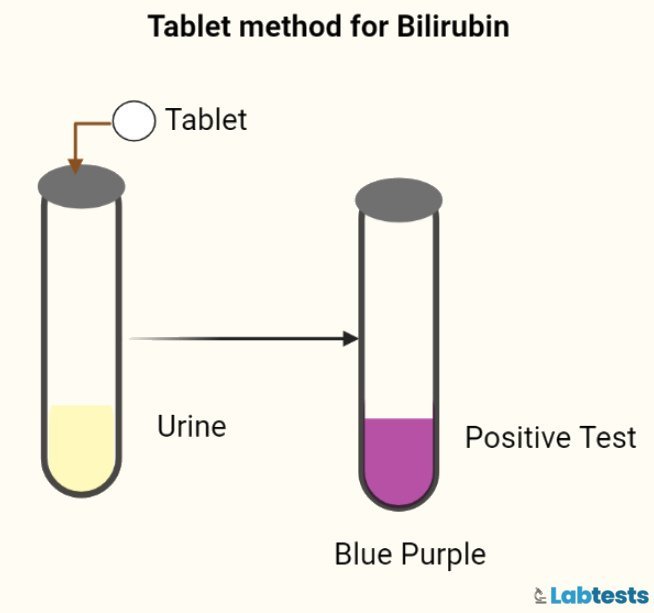
The reagent strip (see figure 7 below) and tablet (see figure 8 below) tests for bilirubin depend on adding bilirubin with a diazonium salt in an acidic medium.
Ictotest tablet test and Reagent Strip Test are examples.
- Tablet method is bilirubin-specific and uses a white dry tablet.
- We can measure a bilirubin level of 0.5 mg/dL in the urine by using the tablet method.
- Strip method uses Diazo reagent and can detect the concentration of 0.5 mg/dL or more.
- Strip method produces a red-violet color.
Indications of Urine Bilirubin test
Following are the indications of bilirubin urine test
- Bilirubin urine test is indicated to diagnose liver conditions like hepatitis or cirrhosis.
- It helps to diagnose liver damage.
- Bilirubin in the urine also indicates that there is a blockage in the excretion of bile.
- Urine test for bilirubin helps to monitor the progress of treatment in hepatitis.
- A bilirubin urine test is indicated when the color of urine becomes abnormal.
- Upon yellowish coloration of the skin, mucous membranes, and sclera, your clinician may ask you for a bilirubin urine test.
Precautions for Urine bilirubin test
Following are the precautions for a bilirubin urine test.
- Avoid mixing the urine sample with stool.
- The sample should be stored at the proper temperature (2-8 degrees).
- Some drugs like phenazopyridine that lead to the red coloration of urine can give a false positive test.
- The test can be falsely negative if a urine sample is stored for a more extended period.
- Bilirubin is sensitive to sunlight, so exposure of the sample to sunlight and patient taking vitamin C in large amounts can also lead to false negative tests.
Clinical significance of Bilirubin urine test
The clinical significance of bilirubin urine test is as follows.
- This test is also helpful when your clinician suspects some liver disease or hemolytic conditions.
- If the bilirubin urine test is positive, it means bilirubin is present in the urine sample, and it’s an early sign of liver damage or obstruction in the excretion of bile from the gallbladder to the intestine.
- Bilirubin is clinically significant and is elevated in diseases like jaundice. Yellowish skin discoloration in jaundice is due to an increased bilirubin level.
- Some drugs like sulfonamides and salicylates dissociate albumin from bilirubin which allows bilirubin to enter the central nervous system and causes neural damage in infants.
What are differential diagnoses for Urinary bilirubin and Urobilinogen?
The following table is helpful to understand the differential diagnosis of urinary bilirubin and urobilinogen
| Test | Normal | Direct/ Conjugated hyperbilirubinemia | Indirect/ Unconjugated hyperbilirubinemia | Direct/ Conjugated hyperbilirubinemia |
| Etiology | Biliary obstruction | Hepatitis | Hemolysis | |
| Urobilinogen | Negative/ positive | Positive (+++) | Increased (Positive) | Absent |
| Urine bilirubin | Negative | Positive | Usually absent | Increased (Positive) |
Frequently asked questions
Q1. What causes an increased level of direct bilirubin?
Direct or conjugated bilirubin is elevated in the following conditions:
• Cirrhosis
• Viral hepatitis
• Alcoholic hepatitis
• Chlorpromazine causing intrahepatic disruption
• Biliary cirrhosis
• Biliary atresia
• Cholangitis
• Gall stones
• Gall bladder tumor
• Bile duct tumor
• Head of the pancreas tumor
• Bile duct stricture formation
Q2. What causes an increased level of indirect bilirubin?
Indirect or unconjugated bilirubin is elevated in the following conditions.
• Spherocytosis
• Hemoglobinopathies
• G6PD deficiency
• Transfusion reaction
• Hemorrhage
• Pernicious anemia
• Inefficient erythropoiesis
• Genetic diseases like Gilbert syndrome
• Viral hepatitis
Q3. What is kernicterus?
Kernicterus is a medical condition in which the bilirubin level is so high in newborn babies that it moves from blood to the brain tissue and accumulates there(5). In brain tissues, it causes permanent injury and damage if not diagnosed or treated on time.
Q4. How do I know that my urine sample has bilirubin?
If the urine sample contains bilirubin in it, the color of the urine will be brown, and it will produce yellow-colored foam when shaken. When voided, urine having bilirubin in it will be red-brown. And it will turn green on standing, especially when exposed to light.
Q5. How can we measure bilirubin?
We can measure the value of bilirubin in blood and urine.
Q6. What are bile pigments?
Bilirubin along with its derivatives is collectively called bile pigments.
References
- Hoilat GJ, John S. Bilirubinuria. [Updated 2022 Aug 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557439/
- Alfred H. Free, Helen M. Free, A Simple Test for Urine Bilirubin, Gastroenterology, Volume 24, Issue 3, 1953, Pages 414-421, ISSN 0016-5085, https://doi.org/10.1016/S0016-5085(53)80143-5.
- Wang, Jayanta Roy Chowdhury, Namita Roy Chowdhury, Bilirubin metabolism: Applied physiology, Current Paediatrics, Volume 16, 2006, Pages 70-74, ISSN 0957-5839, https://doi.org/10.1016/j.cupe.2005.10.002.
- Godfried EG. Clinical tests for bilirubin in urine. Biochem J. 1934;28(6):2056-60. doi: 10.1042/bj0282056. PMID: 16745610; PMCID: PMC1253439.
- Dag Bratlid, How Bilirubin Gets into the Brain, Clinics in Perinatology, Volume 17, Issue 2, 1990, Pages 449-465, ISSN 0095-5108, https://doi.org/10.1016/S0095-5108(18)30578-5.
- Sticova E, Jirsa M. New insights in bilirubin metabolism and their clinical implications. World J Gastroenterol. 2013 Oct 14;19(38):6398-407. doi: 10.3748/wjg.v19.i38.6398. PMID: 24151358; PMCID: PMC3801310.
- Lockwood, Wanda. “The complete urinalysis and urine tests.” (2022).
- Tietz Textbook of Clinical Chemistry and Molecular Diagnostics – 6th Edition. (2017, January 16). Retrieved October 21, 2022, from https://www.elsevier.com/books/tietz-textbook-of-clinical-chemistry-and-molecular-diagnostics/rifai/978-0-323-35921-4
- Kalakonda A, Jenkins BA, John S. Physiology, Bilirubin. [Updated 2022 Sep 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470290/
- Mesić, I., Milas, V., Međimurec, M. i Rimar, Ž. (2014). Unconjugated Pathological Jaundice in Newborns. Collegium antropologicum, 38 (1), 173-178. Preuzeto s https://hrcak.srce.hr/120876