HbA1c is also known as glycated hemoglobin. HbA1c is a blood test used in monitoring and diagnosing diabetes mellitus. It is an excellent screening tool for Diabetes that the ADA (American Diabetes Association) recommends.
When sugar enters the bloodstream, it gets attached to hemoglobin. All of us have some sugar attached to the hemoglobin, but prediabetics or diabetics have more. The HbA1c test will measure the percentage of RBCs having sugar-coated hemoglobin.
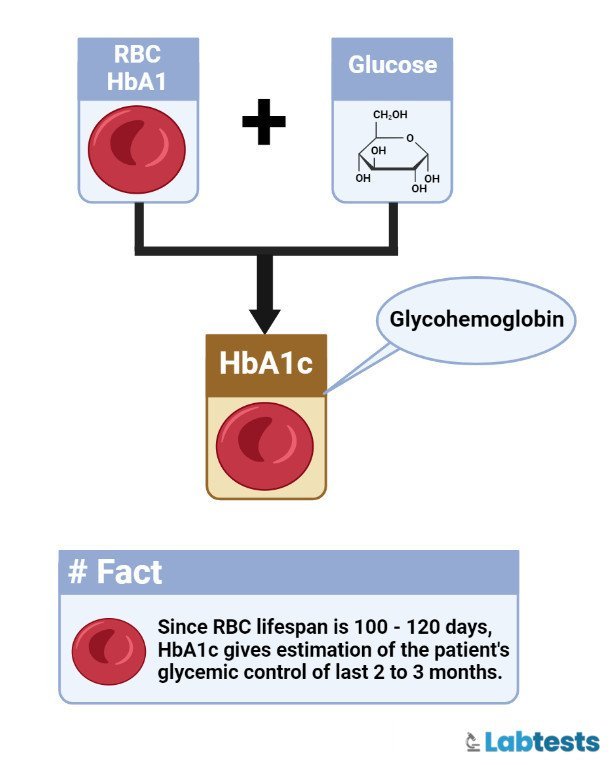
HbA1c is formed when hemoglobin joins the glucose molecule in the blood, called ‘glycated’. HbA1c is the preferred tool for long-term monitoring of glycaemic control in people with Diabetes.
If Diabetes is poorly controlled in diabetics, their average blood glucose concentrations will be high, leading to higher HbA1c concentrations.
Introduction
The HbA1c test is widely used as a diagnostic tool for diabetes mellitus. Diabetes Mellitus is a metabolic disorder characterized by a chronic hyperglycemic state and disturbances of macromolecules like fat, protein, and carbohydrate metabolism due to defective insulin secretion, insulin action, and sometimes both.
Glycated hemoglobin (HbA1c) was introduced into clinical usage in the 1980s and reflected the average glucose level in plasma over the past 2 to 3 months.
Fasting or any special preparation is not needed to test glycated hemoglobin (HbA1c); we can perform it at any time. That’s why it is the preferred test for assessing glycemic control in people with diabetes as a screening method.
The HbA1c test is also a screening test for persons at high risk of Diabetes. It is preferred not to use a finger-prick HbA1c test. Finger prick HbA1c test must be confirmed by laboratory venous HbA1c level in all patients.
People with diabetes are at increased risk of developing cardiac, peripheral arterial, and cerebrovascular diseases. If Diabetes persists for extended periods, it develops retinopathy, nephropathy, and neuropathy.
Normal Value (Range) of HbA1c Chart
According to the World Health Organization (WHO), an HbA1c value of 48 mmol/mol (6.5%) is recommended as the cut point for diagnosing Diabetes Mellitus.
An HbA1c value of less than 48 mmol/mol (6.5%) does not exclude diabetes mellitus that is interpreted using glucose tests.
| Normal Values | Below 5.7% (39 mmol/mol) |
| Pre-diabetes (risk of diabetes) | 5.7% to 6.4% (39 to 46 mmol/mol) |
| Diabetes Mellitus (is diagnosed at this value) | 6.5% (48 mmol/mol) or above |
Correlation between HbA1c and average blood sugar level
Why is relating HbA1c to glucose important?
- For diabetics, glucose monitoring is necessary. Aside from the quarterly lab test, daily glucose monitoring is also done, and many patients are taught how to monitor glucose by themselves (Self-monitoring of blood glucose/SMBG) at home.
- One of the important aspects of self-monitoring of blood glucose is understanding the relationship between HbA1c and glucose, understanding the readings in mg/dl, and what these numbers mean.
- Although HbA1c is a far better gauge in determining how well-controlled a patient’s blood glucose level is.
The correlation between HbA1c (NGSP in % and IFCC in mmol/mmol) and estimated Average Glucose (eAG) level (in mg/dl and mmol/l) is following.
Note :
- NGSP – National Glycohemoglobin Standardization Program (most commonly used units)
- IFCC – International Federation of Clinical Chemistry Working Group (proposed new metric based on methods mass spectroscopy and capillary electrophoresis)
Formula to convert HbA1c to eAG is based on 2 studies – 1. DCCT (Diabetes Control and Complications Trial) study and 2. ADAG (A1c-Derived Average Glucose) study
Reference : http://www.ngsp.org/A1ceAG.asp
- DCCT formula – Results showed a linear relationship between HbA1c and AG (AG(mg/dL) = ( 35.6 x HbA1c ) – 77.3), with a Pearson correlation coefficient (r) of 0.82.
- ADAG Study – The relationship between eAG and HbA1c based on linear regression analysis was: eAG(mg/dl)= (28.7*HbA1c)-46.7, r2=0.84
Formula to convert NGSP and IFCC is (NGSP = [0.09148 * IFCC] + 2.152)
Reference : http://www.ngsp.org/ifcc.asp
| NGSP – HbA1c (%) | IFCC – HbA1c (mmol/mol) | eAG – (mg/dL) | eAG – (mmol/l) |
|---|---|---|---|
| 3 | 9 | 39 | 2.2 |
| 4 | 20 | 68 | 3.8 |
| 5 | 31 | 97 | 5.4 |
| 6 | 42 | 126 | 7.0 |
| 7 | 53 | 154 | 8.6 |
| 8 | 64 | 183 | 10.2 |
| 9 | 75 | 212 | 11.8 |
| 10 | 86 | 240 | 13.3 |
| 11 | 97 | 269 | 14.9 |
| 12 | 108 | 298 | 16.6 |
| 13 | 119 | 326 | 18.1 |
| 14 | 130 | 355 | 19.7 |
| 15 | 140 | 384 | 21.3 |
| 16 | 151 | 413 | 22.9 |
| 17 | 162 | 441 | 24.5 |
| 18 | 173 | 470 | 26.1 |
| 19 | 184 | 499 | 27.7 |
| 20 | 195 | 527 | 29.3 |
You can also check this calculator – for conversion of HbA1c values – http://www.ngsp.org/convert1.asp
Factors effecting HbA1c estimation
The following factors influence HbA1c and its measurements.
Assays:
- Increased HbA1c levels can be due to alcoholism, chronic opiate use, large doses of aspirin, hyperbilirubinemia, and carbamylated hemoglobin.
- Decreased HbA1c can be due to hypertriglyceridemia.
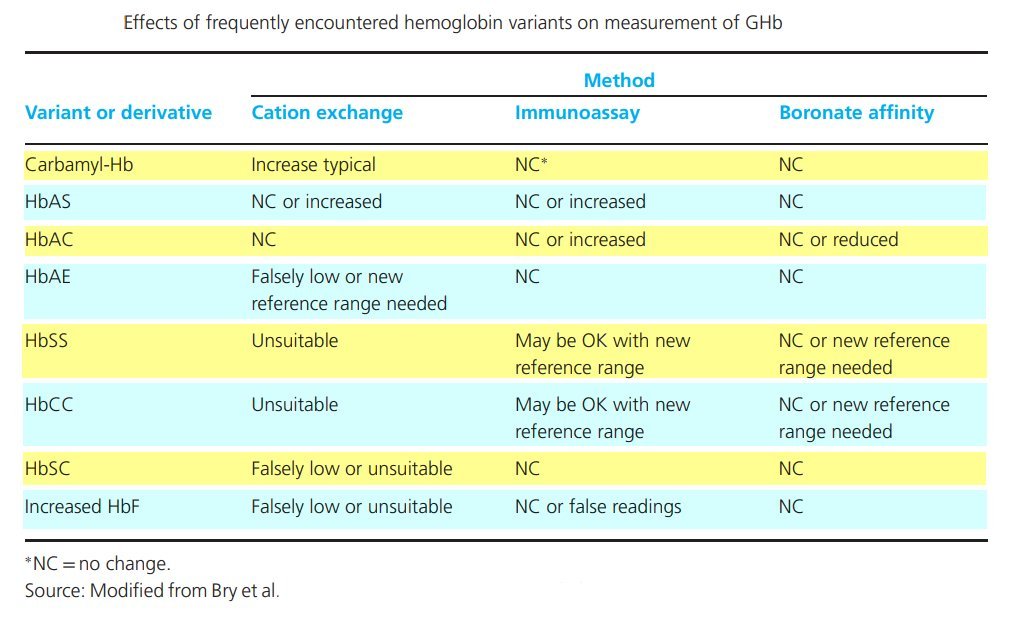
- Variable HbA1c levels can be because of hemoglobinopathies.
Erythropoiesis:
- Increased HbA1c levels can result from iron, vitamin B12 deficiency, and decreased erythropoiesis.
- Decreased HbA1c level is due to the administration of erythropoietin, iron, vitamin B12, reticulocytosis, and chronic liver disease.
Glycation:
- Increased HbA1c levels include alcoholism, chronic renal failure, and decreased intraerythrocytic pH.
- Decreased HbA1c levels due to aspirin, vitamin C, and E, certain hemoglobinopathies, and increased intra-erythrocyte pH.
- Variable HbA1c due to genetic determinants.
Altered Hemoglobin:
- Genetic or chemical alterations in hemoglobin due to hemoglobinopathies, HbF, and methemoglobin may increase or decrease HbA1c.
Erythrocyte destruction:
- Increased HbA1c levels like increased erythrocyte life span, i.e., Splenectomy.
- Decreased A1c, such as decreased erythrocyte life span, i.e., hemoglobinopathies, splenomegaly, rheumatoid arthritis, or drugs such as antiretrovirals, ribavirin, and dapsone.
Summary on various conditions affecting the measurement of Glycated Hb levels by the chromatography method
Falsely High (HbA1c) measured levels
- Lead poisoning
- Chronic aspirin therapy
- Alcoholism
- Hyperbilirubinemia
- Elevated triglycerides
- Iron-deficiency anemia
- Post-splenectomy patients
- Opiate addiction state
- Uremia (carbamylation of Hb)
- Negatively charged hemoglobin variants
Falsely Low (HbA1c) measured levels
- Pregnancy state
- Hemolytic anemias
- Positively charged Hb (hemoglobin) variants
- Blood loss (Acute or chronic)
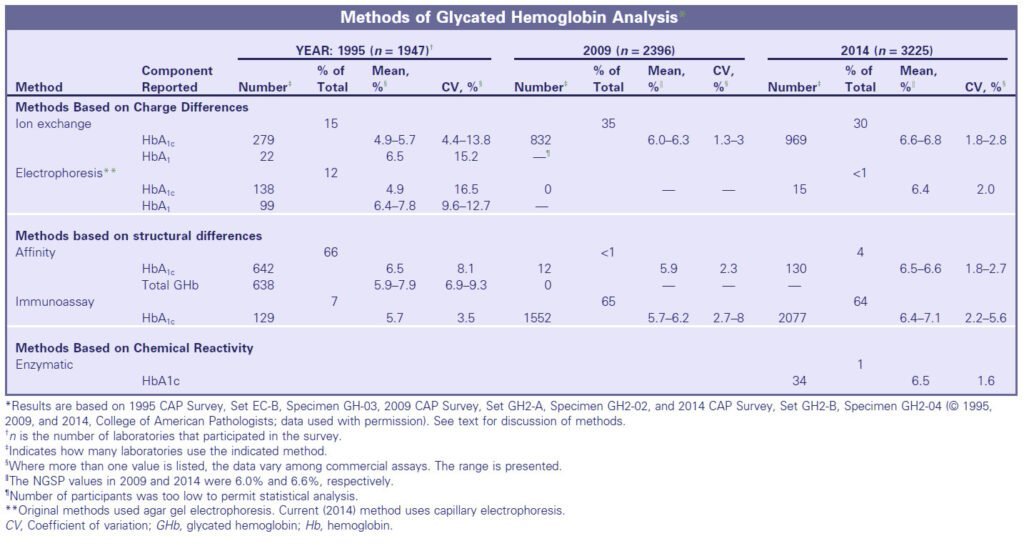
Methods for determination of glycated hemoglobin (HbA1c)
More than 150 different methods are devised to determine glycated hemoglobin. All these methods have various indications. The most common methods used to separate GHb from non-glycated hemoglobin are based on charge differences and include ion-exchange chromatography, HPLC, electrophoresis, and isoelectric focusing.
The methods that use structural differences are affinity chromatography and immunoassay. And the methods that use chemical analysis are enzymatic, photometry, and spectrophotometry. Some of the commercially available methods are the following.
Ion-Exchange Minicolumns:
- Ion-exchange chromatography is used to separate hemoglobin variants based on charge.
- The hemoglobin is charged positively, and the cation-exchange resin is charged negatively.
- These resins are packed in a disposable minicolumn and have an affinity for hemoglobin.
- The sample of the patient is hemolyzed and applied to the column.
- Then a buffer is used, and the eluent is collected.
- The pH of the eluent, along with ionic strength, is selected. Compared to the HbA, GHbs (A1a + A1b + A1c) are eluted first because these don’t bind to the negatively charged resin and are less positively charged than HbA.
- All the forms of GHbs, (A1a + A1b + A1c) are collectively expressed as HbA1.
- These glycated hemoglobins are measured in a spectrophotometer. Then the second buffer is added that is of different ionic strength.
- It will help to elute the more positively charged main hemoglobin fraction.
- GHb is expressed as a percentage of total hemoglobin.
- Most of the current commercial ion-exchange methods use HPLC.
- Thermostatting the column is done because the temperature of the reagents and columns is essential to control if we want accurate and reproducible results.
- The pH and ionic strength should also be controlled strictly. Sample storage conditions are crucial.
High-Performance Liquid Chromatography:
- HPLC can also separate HbA1c. HPLC employs cation-exchange chromatography.
- Automated assays require a sample of only 5 µL of whole blood. Venous blood is commonly used for this purpose.
- If the sample is anticoagulated, dilute it with a hemolysis reagent containing borate.
- It is essential to incubate at 37°C for 30 minutes to remove the Schiff base and then insert it into the autosampler.
- A step gradient using three phosphate buffers of increasing ionic strength is passed through the column.
Immunoassay:
- Assays for HbA1c use antibodies raised against keto-amine linkage plus the first four to eight amino acids at the N-terminal end of the β-chain of hemoglobin.
- Immunoassay for HbA1c measures HbA1c in whole blood by inhibition of latex agglutination.
- Agglutinator is a synthetic polymer with multiple copies of the immunoreactive portion of HbA1c.
- Agglutinator binds with the antiHbA1c monoclonal antibody that is attached to latex beads. This agglutination process creates scattered light. This scattered light is measured as an increase in absorbance.
Affinity Chromatography:
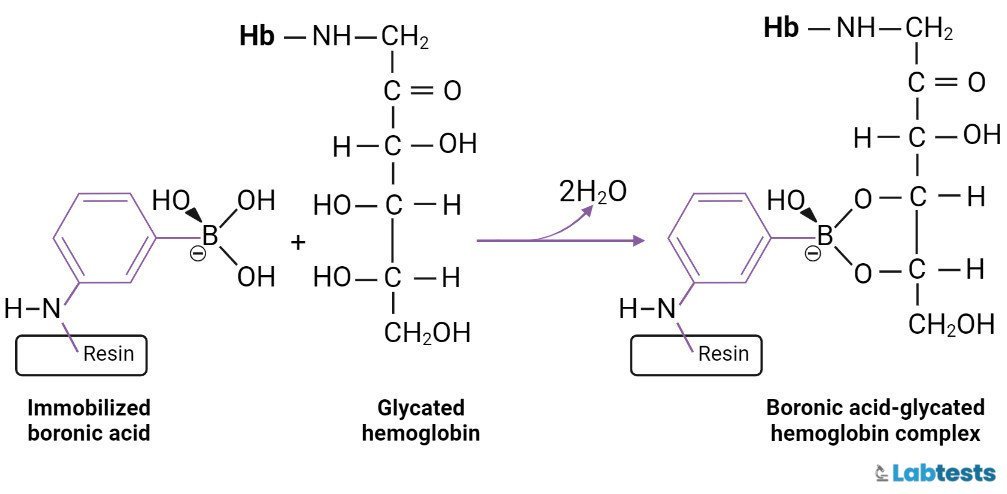
- Affinity gel columns are used to separate glycated hemoglobin from the non-glycated fraction. m-Aminophenylboronic acid is cross-linked to agarose or another matrix (e.g., glass fiber) and gets immobilized.
- The boronic acid binds to Hb and forms a reversible five-member ring complex, thus holding the glycated hemoglobin on the column.
- The non-glycated hemoglobin does not bind. Then sorbitol is added to elute the glycated hemoglobin.
Capillary Electrophoresis:
- Capillary electrophoresis method uses high voltage and high resolving ability. In this technique, charged molecules are separated in an alkaline buffer.
- We can detect hemoglobins by absorption spectroscopy at the cathodic end of the capillary.
Enzymatic Assays:
- Enzymatic assays are also developed to measure HbA1c. This technique catalyzes oxidative deglycation of N-(deoxy fructosyl)-Val-His by fructosyl peptide oxidase.
- FDA approves enzymatic assays in the United States. A kit is commercially available and can be used on many automated analyzers.
Summary
Specimen collection and storage
- No need to fast.
- Venous blood is required for sampling
- The sample will be taken in a tube containing EDTA or Oxalate with fluoride.
- Whole blood can be stored at 4℃ for up to 07 days.
- For the ion exchange method, it is recommended not to store the sample at -20℃.
- The heparinized blood sample is needed to be assayed within 48 hours.
WHO criteria for the diagnosis of Diabetes Mellitus
There are four diagnostic tests for diabetes mellitus that are currently recommended.
- Fasting plasma glucose
- An oral glucose tolerance test (OGTT) is 2-hour postload plasma glucose after a 75 g glucose
- HbA1c
- Random blood sugar level when there are signs and symptoms of Diabetes.
People will be considered diabetic if fasting plasma glucose level is ≥ 7.0 mmol/L (126 mg/dl), 2-hour post-load plasma glucose is ≥ 11.1 mmol/L (200 mg/dl), HbA1c level is ≥ 48 mmol/mol ( 6.5%), or a random blood glucose level is ≥ 11.1 mmol/L (200 mg/ dl) when there are signs and symptoms present.
If an asymptomatic person has elevated values, it is advised to repeat the test, preferably with the same test, on a subsequent day to confirm the diagnosis.
Frequently asked questions
Q1. What are the advantages of affinity chromatography?
• Hemoglobin variants like HbS, HbC, HbD, or HbE produce a minimal effect.
• No interference from non-glycated hemoglobins.
• Minimum interference from the labile intermediate form of HbA1c
• Variations in temperature don’t affect
• It’s precise.
Q2. What are the limitations of using immunoassay?
• Antibodies do not recognize other Glycated hemoglobins like HbA1a or HbA1b.
• Several hemoglobin variants, like HbF, HbA2, HbS, and carbamylated hemoglobin, are also not detected.
Q3. How is HbA1c tested?
HbA1c value is measured through a blood sample. Usually, the whole blood sample is used for this test. Venous blood is collected, stored, and analyzed through an automated analyzer.
Q4. What does it mean if the HbA1c level is high?
If the HbA1c level is 6.5% or higher, it is called Diabetes, which means you have too much sugar in your blood. Having uncontrolled diabetes affects your organs like kidneys, eyes, and feet. Some severe complications can be due to this.
Q5. What is the normal HbA1c level?
If the person does not have Diabetes, the normal range for the HbA1c is 4% to 5.6%. If the value of HbA1c is between 5.7% and 6.4%, we call it the prediabetic stage. And if the value of HbA1c is 6.5% or higher, it indicates that you have diabetes.
Q6. In which situations HbA1c test is not appropriate for the diagnosis of Diabetes?
The HbA1c test is not appropriate for the diagnosis of Diabetes in the following situations
• In Type 1 diabetes
• In patients at high risk who require hospital admission and are acutely ill
• In all children and young adults
• In patients with acute pancreatic damage, it can be pancreatic surgery.
• In pregnant females.
• In patients taking medication like steroids, and antipsychotics. These may cause rapid glucose rise.
• In patients having symptoms of Diabetes Mellitus for less than two months
Q7. What is the best time for hba1c test ?
HbA1c testing can be given at any time of the day and doesn’t require fasting. There is no preparation required for this test.
Content reviewed by Endocrinologist – Dr. Rajesh Moganti MBBS, M.D, DM
References
- World Health Organization. Definition, Diagnosis, and Classification of Diabetes Mellitus and its Complications. Part 1: Diagnosis and Classification of Diabetes Mellitus. WHO/NCD/NCS/99.2 ed. Geneva, World Health Organization, 1999.
- All About Your A1C. (2018, August 21). Centers for Disease Control and Prevention. https://www.cdc.gov/diabetes/managing/managing-blood-sugar/a1c.html
- Tietz Textbook of Clinical Chemistry and Molecular Diagnostics – 6th Edition. (2017, January 16). Retrieved October 21, 2022, from https://www.elsevier.com/books/tietz-textbook-of-clinical-chemistry-and-molecular-diagnostics/rifai/978-0-323-35921-4